Platelet-Rich Plasma For Arthritis
Platelet-rich plasma (PRP) uses a component of a person’s own blood to treat their osteoarthritis. PRP is a safe treatment which gives significant benefit to people suffering from osteoarthritis including improvements in stiffness, pain and mobility.

Regenerative
PRP injections boost growth factor concentration locally, enhancing tissue repair, improving pain and improving the overall integrity of the joint. The best results are typically seen within 6-8 weeks.
High Success Rate
A PRP injection is a highly effective treatment supported by a large body of scientific evidence. PRP has been found to be more effective than cortisone or hyaluronic acid injections.
Lasting Results
Results from PRP can last for months to years. Severity of osteoarthritis and bodyweight play a role in how long results last. Patients are typically very satisfied with results.
Platelet-Rich Plasma
Regenerative injection treatment
Getting Started With Platelet-Rich Plasma
To ensure that platelet-rich plasma will be a safe and effective treatment for you an initial naturopathic consultation is required prior to starting treatment. The initial platelet-rich plasma treatment is offered at a lesser cost if it is on the same day as the initial consultation.
Initial visit: $180
Subsequent platelet-rich plasma treatment: $450
Initial visit with platelet-rich plasma treatment: $500 ($130 savings)
Growth Factors Promote Repair
PRP injections contain a high concentration of your own platelets. These platelets contain a large amount of growth factors, including platelet-derived growth factor (PDGF), transforming growth factor beta (TGF-β), insulin-like growth factor (IGF), epidermal growth factor (EGF) and vascular endothelial growth factor (VEGF)1.
| Growth Factor | Effect on Tissue Repair |
| EGF | Stimulates cellular proliferation |
| IGF | Mediates growth and repair of skeletal muscle |
| PDGF | Encourages proliferation of fibroblasts, enhances collagen synthesis |
| TGF-β | Stimulates fibroblast proliferation, formation of collagen, and extracellular matrix components |
| VEGF | Promotes angiogenesis |
These growth factors trigger tissue repair in our natural healing and recovery process. When a high concentration of these growth factors is introduced into the area of an injured or arthritic joint the healing process is jump-started.
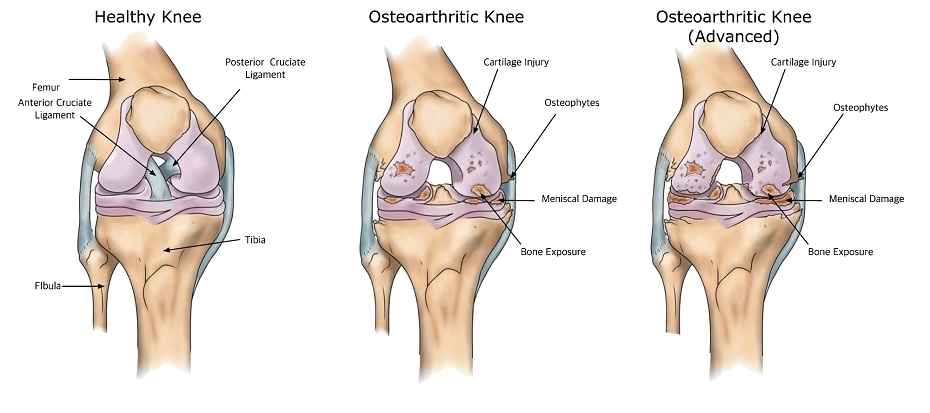
Some research has suggested that PRP improves the integrity of the joint cartilage by increasing the amount of cartilage producing cells (chondrocytes) and by decreasing their rate of cell death (apoptosis)3. This would conceivably lead to a larger number of chondrocytes actively producing healthy cartilage within the joint and a healthier joint as a result.
How Is Platelet-Rich Plasma Prepared?

PRP is prepared by drawing and centrifuging a small sample of your own blood on the day of treatment. A centrifuge is a device which rapidly rotates, spinning a blood sample at a high speed causing it to separate into layers based on weight. After centrifugation the blood sample separates into a top layer of plasma which is transparent yellow in colour (mostly water with some dissolved proteins) and a bottom thick, red layer (red blood cells). At the junction of the plasma and red blood cell layers sits a dense concentration of platelets. This platelet-rich layer of the plasma is the portion of the blood which is collected and used for injection.
How Is Platelet-Rich Plasma Administered?

PRP is given by injection into the affected site or the site of injury. For example, in cases of tennis elbow the PRP injection is made at the site of the affected common extensor tendon on the elbow and in plantar fasciitis the injection is given at the site of the damaged plantar fascia insertion on the heel of the foot. In the case of osteoarthritis the “injury” includes two entire joint surfaces. An osteoarthritic joint is treated by injecting PRP into an affected joint space. Since a joint is a closed compartment the PRP fluid stays within the joint, coating the affected joint surfaces and exerting its effect on them through its rich concentration of growth factors.
Effectiveness Of Platelet-Rich Plasma For Osteoarthritis
Many studies have been performed on PRP injections for osteoarthritis and the results have been near-unanimously positive, showing a reduction in pain and improvement in mobility among the people receiving the treatment. In total, 54 studies have investigated PRP as a treatment for osteoarthritis and all 54 of these studies have found that this treatment was beneficial4-57.
Some research has found that 3 PRP injections, with 1 month between each injection, is more effective and gives longer lasting results than only one or two injections33.
Platelet-rich plasma vs hyaluronic acid:
- 24 studies have compared PRP treatment to injections of hyaluronic acid for osteoarthritis.34-57
- 20 of these 24 studies found PRP was a better treatment than hyaluronic acid37-56.
- 3 of these 24 studies found that PRP is as good as hyaluronic acid treatment34-36.
- 1 of these 24 studies found that hyaluronic was a better treatment than PRP57.
Which Joints Are Helped?
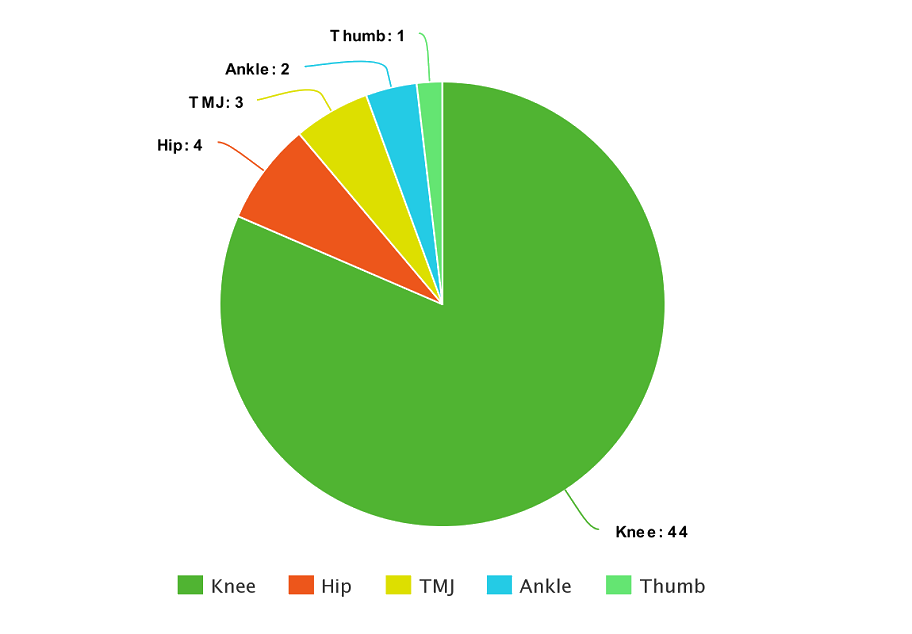
Figure 1. Number of studies (by joint) examining platelet-rich plasma for osteoarthritis. Most research performed on knee joint
Most PRP for osteoarthritis research has been on the knee. To date 44 studies have examined PRP’s effect on knee osteoarthritis while the hip has 4 studies, the temporomandibular joint has 3 studies, the ankle has 2 studies and the thumb has 1 study.
Although the studies have yet to be done I have also seen good results with osteoarthritis of other joints including the shoulder, wrist and other hand joints.
Safety
PRP injection treatments are quite safe, having very little in the way of reported adverse effects58. While most treatments for pain involve a synthetic medication-based therapy, PRP simply uses a component of a person’s blood. PRP therefore carries very little risk of causing an allergic reaction. The most common adverse effect of PRP is discomfort at the site of treatment for 1-3 days. This is a common reaction as the mechanism of action of PRP involves a short-term inflammatory phase after treatment which can contribute to discomfort temporarily. As with any injection there is a small chance of infection. There is also a small chance of allergic reaction to the local anesthetic (numbing agent) which is used at the site of the injection.
People with active cancer or active infection are not candidates for PRP treatment. People with thrombocytopenia (low platelets) and people on blood thinners can have PRP treatment but some changes to the treatment may be required.
What To Expect Before & After Treatment
PRP treatment can provide lasting results for people with osteoarthritis including reduced pain and improved mobility. Typically 3 treatments will be required to attain maximum benefit from PRP. PRP injections can be done 2-4 weeks apart without issue.
PRP injections are a long-term solution for osteoarthritis. While this treatment gives long term benefit some people may experience discomfort following treatment for 1-3 days. In order to deal with this possible discomfort it is best to reduce physical activity after a PRP injection to avoid additional discomfort of the region which was treated. Applying ice to the affected area will not inhibit the effectiveness of the PRP treatment and may help if the treated area is achy or sore.
The treated body part should be rested on the day of treatment and if discomfort remains then 2-3 days of avoiding heavy activity may be required to assist in recovering. Anti-inflammatories such as aspirin, ibuprofen and naproxen in general should not be taken for 2-7 days after a PRP treatment as they could theoretically dampen its effectiveness. Generally acetaminophen (Tylenol) is preferable to anti-inflammatories in this short term to manage any discomfort or pain which may be present.
Frequently Asked Questions
Platelet-rich plasma injections may cause minor discomfort, but this sensation is generally brief. The needle used in these treatments is smaller than those utilized for blood draws or cortisone injections. To further alleviate discomfort, a local anesthetic agent is included in the platelet-rich plasma procedure.
Three treatment sessions at a rate of one injection every two weeks yields optimal results for osteoarthritis.
After a platelet-rich plasma treatment it is best to limit exercise to less intense activities for 1-2 days to allow the treated region to complete the repair process unhindered.
You may not be a candidate for platelet-rich plasma treatment if you are pregnant, have had a knee replacement, or have post-infectious arthritis.
References
- Lubkowska A, Dolegowska B, Banfi G. Growth factor content in PRP and their applicability in medicine. J Biol Regul Homeost Agents. 2012 Apr-Jun;26(2 Suppl 1):3S-22S.
- Middleton KK, Barro V, Muller B, et al. Evaluation of the effects of platelet-rich plasma (PRP) therapy involved in the healing of sports-related soft tissue injuries. Iowa Orthop J. 2012;32:150-163.
- Moussa M, Lajeunesse D, Hilal G, El Atat O, Haykal G, Serhal R, Chalhoub A, Khalil C, Alaaeddine N. Platelet rich plasma (PRP) induces chondroprotection via increasing autophagy, anti-inflammatory markers, and decreasing apoptosis in human osteoarthritic cartilage. Exp Cell Res. 2017 Mar 1;352(1):146-156.
- Acosta-Olivo C, Esponda-Colmenares F, Vilchez-Cavazos F, Lara-Arias J, Mendoza-Lemus O, Ramos-Morales T. Platelet rich plasma versus oral paracetamol for the treatment of early knee osteoarthritis. Preliminary study. Cir Cir. 2014 Mar-Apr;82(2):163-9.
- Repetto I, Biti B, Cerruti P, Trentini R, Felli L. Conservative Treatment of Ankle Osteoarthritis: Can Platelet-Rich Plasma Effectively Postpone Surgery? J Foot Ankle Surg. 2017 Mar – Apr;56(2):362-365.
- Joshi Jubert N, Rodríguez L, Reverté-Vinaixa MM, Navarro A. Platelet-Rich Plasma Injections for Advanced Knee Osteoarthritis: A Prospective, Randomized, Double-Blinded Clinical Trial. Orthop J Sports Med. 2017 Feb 13;5(2):2325967116689386.
- Fukawa T, Yamaguchi S, Akatsu Y, Yamamoto Y, Akagi R, Sasho T. Safety and Efficacy of Intra-articular Injection of Platelet-Rich Plasma in Patients With Ankle Osteoarthritis. Foot Ankle Int. 2017 Apr 1:1071100717700377.
- Chen CPC, Cheng CH, Hsu CC, Lin HC, Tsai YR, Chen JL. The influence of platelet rich plasma on synovial fluid volumes, protein concentrations, and severity of pain in patients with knee osteoarthritis. Exp Gerontol. 2017 Jul;93:68-72.
- Cömert Kiliç S, Güngörmüş M, Sümbüllü MA. Is Arthrocentesis Plus Platelet-Rich Plasma Superior to Arthrocentesis Alone in the Treatment of Temporomandibular Joint Osteoarthritis? A Randomized Clinical Trial. J Oral Maxillofac Surg. 2015 Aug;73(8):1473-83.
- Hart R, Safi A, Komzák M, Jajtner P, Puskeiler M, Hartová P. Platelet-rich plasma in patients with tibiofemoral cartilage degeneration. Arch Orthop Trauma Surg. 2013 Sep;133(9):1295-301.
- Jang SJ, Kim JD, Cha SS. Platelet-rich plasma (PRP) injections as an effective treatment for early osteoarthritis. Eur J Orthop Surg Traumatol. 2013 Jul;23(5):573-80.
- Patel S, Dhillon MS, Aggarwal S, Marwaha N, Jain A. Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial. Am J Sports Med. 2013 Feb;41(2):356-64.
- Filardo G, Kon E, Pereira Ruiz MT, Vaccaro F, Guitaldi R, Di Martino A, Cenacchi A, Fornasari PM, Marcacci M. Platelet-rich plasma intra-articular injections for cartilage degeneration and osteoarthritis: single- versus double-spinning approach. Knee Surg Sports Traumatol Arthrosc. 2012 Oct;20(10):2082-91.
- Sampson S, Reed M, Silvers H, Meng M, Mandelbaum B. Injection of platelet-rich plasma in patients with primary and secondary knee osteoarthritis: a pilot study. Am J Phys Med Rehabil. 2010 Dec;89(12):961-9.
- Simental-Mendía M, Vílchez-Cavazos JF, Peña-Martínez VM, Said-Fernández S, Lara-Arias J, Martínez-Rodríguez HG. Leukocyte-poor platelet-rich plasma is more effective than the conventional therapy with acetaminophen for the treatment of early knee osteoarthritis. Arch Orthop Trauma Surg. 2016 Aug 9.
- Loibl M, Lang S, Dendl LM, Nerlich M, Angele P, Gehmert S, Huber M. Leukocyte-Reduced Platelet-Rich Plasma Treatment of Basal Thumb Arthritis: A Pilot Study. Biomed Res Int. 2016;2016:9262909.
- Sánchez M, Delgado D, Sánchez P, Muiños-López E, Paiva B, Granero-Moltó F, Prósper F, Pompei O, Pérez JC, Azofra J, Padilla S, Fiz N. Combination of Intra-Articular and Intraosseous Injections of Platelet Rich Plasma for Severe Knee Osteoarthritis: A Pilot Study. Biomed Res Int. 2016;2016:4868613.
- Sánchez M, Guadilla J, Fiz N, Andia I. Ultrasound-guided platelet-rich plasma injections for the treatment of osteoarthritis of the hip. Rheumatology (Oxford). 2012 Jan;51(1):144-50.
- Smith PA. Intra-articular Autologous Conditioned Plasma Injections Provide Safe and Efficacious Treatment for Knee Osteoarthritis: An FDA-Sanctioned, Randomized, Double-blind, Placebo-controlled Clinical Trial. Am J Sports Med. 2016 Apr;44(4):884-91.
- Gobbi A, Lad D, Karnatzikos G. The effects of repeated intra-articular PRP injections on clinical outcomes of early osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2015 Aug;23(8):2170-7.
- Kavadar G, Demircioglu DT, Celik MY, Emre TY. Effectiveness of platelet-rich plasma in the treatment of moderate knee osteoarthritis: a randomized prospective study. J Phys Ther Sci. 2015 Dec;27(12):3863-7.
- Rayegani SM, Raeissadat SA, Taheri MS, Babaee M, Bahrami MH, Eliaspour D, Ghorbani E. Does intra articular platelet rich plasma injection improve function, pain and quality of life in patients with osteoarthritis of the knee? A randomized clinical trial. Orthop Rev (Pavia). 2014 Sep 18;6(3):5405.
- Torrero JI, Aroles F, Ferrer D. Treatment of knee chondropathy with platelet rich plasma. Preliminary results at 6 months of follow-up with only one injection. J Biol Regul Homeost Agents. 2012 Apr-Jun;26(2 Suppl 1):71S-78S.
- Halpern B, Chaudhury S, Rodeo SA, Hayter C, Bogner E, Potter HG, Nguyen. Clinical and MRI outcomes after platelet-rich plasma treatment for knee osteoarthritis. J. Clin J Sport Med. 2013 May;23(3):238-9.
- Wang-Saegusa A, Cugat R, Ares O, Seijas R, Cuscó X, Garcia-Balletbó M. Infiltration of plasma rich in growth factors for osteoarthritis of the knee short-term effects on function and quality of life. Arch Orthop Trauma Surg. 2011 Mar;131(3):311-7.
- Kon E, Buda R, Filardo G, Di Martino A, Timoncini A, Cenacchi A, Fornasari PM, Giannini S, Marcacci M. Platelet-rich plasma: intra-articular knee injections produced favorable results on degenerative cartilage lesions. Knee Surg Sports Traumatol Arthrosc. 2010 Apr;18(4):472-9.
- Riboh JC, Saltzman BM, Yanke AB, Fortier L, Cole BJ. Effect of Leukocyte Concentration on the Efficacy of Platelet-Rich Plasma in the Treatment of Knee Osteoarthritis. Am J Sports Med. 2016 Mar;44(3):792-800.
- Guler O, Mutlu S, Isyar M, Seker A, Kayaalp ME, Mahirogullari M. Comparison of short-term results of intraarticular platelet-rich plasma (PRP) and hyaluronic acid treatments in early-stage gonarthrosis patients. Eur J Orthop Surg Traumatol. 2015 Apr;25(3):509-13.
- Forogh B, Mianehsaz E, Shoaee S, Ahadi T, Raissi GR, Sajadi S. Effect of single injection of platelet-rich plasma in comparison with corticosteroid on knee osteoarthritis: a double-blind randomized clinical trial. J Sports Med Phys Fitness. 2016 Jul-Aug;56(7-8):901-8.
- Paterson KL, Nicholls M, Bennell KL, Bates D. Intra-articular injection of photo-activated platelet-rich plasma in patients with knee osteoarthritis: a double-blind, randomized controlled pilot study. BMC Musculoskelet Disord. 2016 Feb 9;17:67.
- Sánchez M, Anitua E, Azofra J, Aguirre JJ, Andia I. Intra-articular injection of an autologous preparation rich in growth factors for the treatment of knee OA: a retrospective cohort study. Clin Exp Rheumatol. 2008 Sep-Oct;26(5):910-3.
- Zhang H, Bai Y, Liu C, Jin S, Su K, Liu Y, Lü Z. [Effect of intra-articular injection of platelet-rich plasma on interleukin-17 expression in synovial fluid and venous plasma of knee osteoarthritis patients]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2017 Aug 1;31(8):918-921. [Article in Chinese; Abstract available in Chinese from the publisher]
- Huang PH, Wang CJ, Chou WY, Wang JW, Ko JY. Short-term clinical results of intra-articular PRP injections for early osteoarthritis of the knee. Int J Surg. 2017 Jun;42:117-122.
- Battaglia M, Guaraldi F, Vannini F, Rossi G, Timoncini A, Buda R, Giannini S. Efficacy of ultrasound-guided intra-articular injections of platelet-rich plasma versus hyaluronic acid for hip osteoarthritis. Orthopedics. 2013 Dec;36(12):e1501-8.
- Filardo G, Kon E, Di Martino A, Di Matteo B, Merli ML, Cenacchi A, Fornasari PM, Marcacci M. Platelet-rich plasma vs hyaluronic acid to treat knee degenerative pathology: study design and preliminary results of a randomized controlled trial. BMC Musculoskelet Disord. 2012 Nov 23;13:229.
- Filardo G, Di Matteo B, Di Martino A, Merli ML, Cenacchi A, Fornasari P, Marcacci M, Kon E. Platelet-Rich Plasma Intra-articular Knee Injections Show No Superiority Versus Viscosupplementation: A Randomized Controlled Trial. Am J Sports Med. 2015 Jul;43(7):1575-82.
- Saturveithan C, Premganesh G, Fakhrizzaki S, Mahathir M, Karuna K, Rauf K, William H, Akmal H, Sivapathasundaram N, Jaspreet K. Intra-articular Hyaluronic Acid (HA) and Platelet Rich Plasma (PRP) injection versus Hyaluronic acid (HA) injection alone in Patients with Grade III and IV Knee Osteoarthritis (OA): A Retrospective Study on Functional Outcome. Malays Orthop J. 2016 Jul;10(2):35-40.
- Say F, Gürler D, Yener K, Bülbül M, Malkoc M. Platelet-rich plasma injection is more effective than hyaluronic acid in the treatment of knee osteoarthritis. Acta Chir Orthop Traumatol Cech. 2013;80(4):278-83.
- Hegab AF, Ali HE, Elmasry M, Khallaf MG. Platelet-Rich Plasma Injection as an Effective Treatment for Temporomandibular Joint Osteoarthritis. J Oral Maxillofac Surg. 2015 Sep;73(9):1706-13.
- Cerza F, Carnì S, Carcangiu A, Di Vavo I, Schiavilla V, Pecora A, De Biasi G, Ciuffreda M. Comparison between hyaluronic acid and platelet-rich plasma, intra-articular infiltration in the treatment of gonarthrosis. Am J Sports Med. 2012 Dec;40(12):2822-7.
- Spaková T, Rosocha J, Lacko M, Harvanová D, Gharaibeh A. Treatment of knee joint osteoarthritis with autologous platelet-rich plasma in comparison with hyaluronic acid. Am J Phys Med Rehabil. 2012 May;91(5):411-7.
- Li M, Zhang C, Ai Z, Yuan T, Feng Y, Jia W. Therapeutic effectiveness of intra-knee-articular injection of platelet-rich plasma on knee articular cartilage degeneration. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2011 Oct;25(10):1192-6.
- Kon E, Mandelbaum B, Buda R, Filardo G, Delcogliano M, Timoncini A, Fornasari PM, Giannini S, Marcacci M. Platelet-rich plasma intra-articular injection versus hyaluronic acid viscosupplementation as treatments for cartilage pathology: from early degeneration to osteoarthritis. Arthroscopy. 2011 Nov;27(11):1490-501.
- Lana JF, Weglein A, Sampson SE, Vicente EF, Huber SC, Souza CV, Ambach MA, Vincent H, Urban-Paffaro A, Onodera CM, Annichino-Bizzacchi JM, Santana MH, Belangero WD. Randomized controlled trial comparing hyaluronic acid, platelet-rich plasma and the combination of both in the treatment of mild and moderate osteoarthritis of the knee. J Stem Cells Regen Med. 2016 Nov 29;12(2):69-78.
- Cole BJ, Karas V, Hussey K, Pilz K Fortier LA. Hyaluronic Acid Versus Platelet-Rich Plasma: A Prospective, Double-Blind Randomized Controlled Trial Comparing Clinical Outcomes and Effects on Intra-articular Biology for the Treatment of Knee Osteoarthritis. Am J Sports Med. 2017 Feb;45(2):339-346.
- Fernández-Ferro M, Fernández-Sanromán J, Blanco-Carrión A, Costas-López A, López-Betancourt A, Arenaz-Bua J, Stavaru Marinescu B. Comparison of intra-articular injection of plasma rich in growth factors versus hyaluronic acid following arthroscopy in the treatment of temporomandibular dysfunction: A randomised prospective study. J Craniomaxillofac Surg. 2017 Apr;45(4):449-454.
- Saturveithan C, Premganesh G, Fakhrizzaki S, Mahathir M, Karuna K, Rauf K, William H, Akmal H, Sivapathasundaram N, Jaspreet K. Intra-articular Hyaluronic Acid (HA) and Platelet Rich Plasma (PRP) injection versus Hyaluronic acid (HA) injection alone in Patients with Grade III and IV Knee Osteoarthritis (OA): A Retrospective Study on Functional Outcome. Malays Orthop J. 2016 Jul;10(2):35-40.
- Montañez-Heredia E, Irízar S, Huertas PJ, Otero E, Del Valle M, Prat I, Díaz-Gallardo MS, Perán M, Marchal JA, Hernandez-Lamas, Mdel C. Intra-Articular Injections of Platelet-Rich Plasma versus Hyaluronic Acid in the Treatment of Osteoarthritic Knee Pain: A Randomized Clinical Trial in the Context of the Spanish National Health Care System. Int J Mol Sci. 2016 Jul 2;17(7). pii: E1064.
- Duymus TM, Mutlu S, Dernek B, Komur B, Aydogmus S, Kesiktas FN. Choice of intra-articular injection in treatment of knee osteoarthritis: platelet-rich plasma, hyaluronic acid or ozone options. Knee Surg Sports Traumatol Arthrosc. 2016 Apr 7.
- Sánchez M, Fiz N, Azofra J, Usabiaga J, Aduriz Recalde E, Garcia Gutierrez A, Albillos J, Gárate R, Aguirre JJ, Padilla S, Orive G, Anitua E. A randomized clinical trial evaluating plasma rich in growth factors (PRGF-Endoret) versus hyaluronic acid in the short-term treatment of symptomatic knee osteoarthritis. Arthroscopy. 2012 Aug;28(8):1070-8.
- Lisi C, Perotti C, Scudeller L, Sammarchi L, Dametti F, Musella V, Di Natali G. Treatment of knee osteoarthritis: platelet-derived growth factors vs. hyaluronic acid. A randomized controlled trial. Clin Rehabil. 2017 Aug 1:269215517724193.
- Dallari D, Stagni C, Rani N, Sabbioni G, Pelotti P, Torricelli P, Tschon M, Giavaresi G. Ultrasound-Guided Injection of Platelet-Rich Plasma and Hyaluronic Acid, Separately and in Combination, for Hip Osteoarthritis: A Randomized Controlled Study. Am J Sports Med. 2016 Mar;44(3):664-71.
- Görmeli G, Görmeli CA, Ataoglu B, Çolak C, Aslantürk O, Ertem K. Multiple PRP injections are more effective than single injections and hyaluronic acid in knees with early osteoarthritis: a randomized, double-blind, placebo-controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017 Mar;25(3):958-965.
- Ahmad HS, Farrag SE, Okasha AE, Kadry AO, Ata TB, Monir AA, Shady I. Clinical outcomes are associated with changes in ultrasonographic structural appearance after platelet-rich plasma treatment for knee osteoarthritis. Int J Rheum Dis. 2018 May;21(5):960-966.
- Buendía-López D, Medina-Quirós M, Fernández-Villacañas Marín MÁ. Clinical and radiographic comparison of a single LP-PRP injection, a single hyaluronic acid injection and daily NSAID administration with a 52-week follow-up: a randomized controlled trial. J Orthop Traumatol. 2018 Aug 20;19(1):3.
- Yu W, Xu P, Huang G, Liu L. Clinical therapy of hyaluronic acid combined with platelet-rich plasma for the treatment of knee osteoarthritis. Exp Ther Med. 2018 Sep;16(3):2119-2125.
- Di Sante L, Villani C, Santilli V, Valeo M, Bologna E, Imparato L, Paoloni M, Iagnocco A. Intra-articular hyaluronic acid vs platelet-rich plasma in the treatment of hip osteoarthritis. Med Ultrason. 2016 Dec 5;18(4):463-468.
- Andia I, Maffulli N. Biological Therapies in Regenerative Sports Medicine. Sports Med. 2016 Sep 28.