
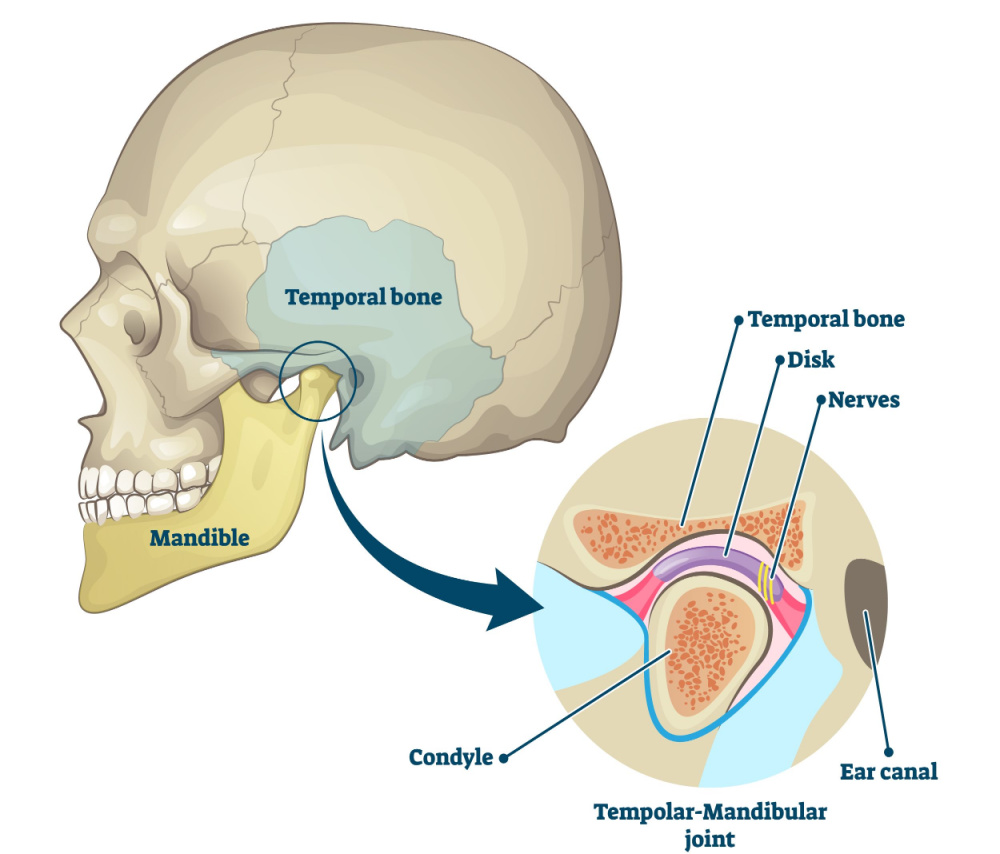
Temporomandibular joint (TMJ) dysfunction is a disorder that affects the jaw joint, causing pain and discomfort in the jaw, face, neck and head. TMJ dysfunction is a common problem, with an estimated 11 million North Americans affected.
The temporomandibular joint is a hinge joint that connects the lower jaw (mandible) to the temporal bone of the skull. It is a complex joint, with multiple components including muscles, ligaments, bones, and cartilage. The specific components of the joint include the joint capsule, articular disc, mandibular condyles, articular surface of the temporal bone, temporomandibular ligament, sphenomandibular ligament, stylomandibular ligament and the lateral pterygoid muscle.
Symptoms Of TMJ Dysfunction
Generally, the most common symptom of TMJ dysfunction is pain and tenderness in the jaw area, especially when opening the mouth or chewing. Other symptoms may include headaches, earaches, clicking or popping noises in the jaw joint, difficulty opening the mouth fully, and locking of the jaw.
Risk Factors For TMJ Dysfunction
Risk factors for TMJ dysfunction can be divided into two categories – physical and psychological. Physical risk factors for TMJ dysfunction include malocclusion of the teeth (not having the top and bottom teeth fit together correctly), grinding of the teeth, trauma to the jaw, arthritis and wearing a dental appliance such as a mouthguard.
Stress, anxiety and depression are psychological risk factors for TMJ dysfunction. Psychological stress and mental health problems can lead to clenching and grinding of the teeth, which can cause wear and tear on the temporomandibular joint. It is important to note that not everyone with these risk factors will develop TMJ dysfunction. If you are experiencing any of the symptoms of TMJ dysfunction, it is important to seek medical attention to get an accurate diagnosis and appropriate treatment.
Treatments For TMJ Dysfunction
Treatments for Temporomandibular Joint (TMJ) dysfunction can be divided into two broad categories: conservative treatments and surgical treatments.
Conservative treatments focus on reducing the symptoms of TMJ dysfunction without resorting to surgery. These treatments may include lifestyle changes such as avoiding hard or chewy foods, managing teeth grinding (bruxism), and taking over-the-counter pain medications such as ibuprofen or acetaminophen. Targeted exercise-based treatments can help to condition the muscles surrounding the temporomandibular joint which can help pain and improve the range of motion of the joint.
Surgical treatment may include arthrocentesis, which involves draining excess fluid from the joint; arthroscopy, which involves using a tiny camera and specialized tools to access the joint and make repairs; and joint replacement surgery, which involves removing the damaged joint and replacing it with an artificial joint. No matter which type of treatment is chosen for TMJ dysfunction, the goal is to reduce pain, improve range of motion, and improve overall quality of life.
Naturopathic Treatment For TMJ Dysfunction
Prolotherapy and platelet-rich plasma (PRP) have both been used as treatment for temporomandibular joint (TMJ) dysfunction. Prolotherapy is an injection of a concentrated dextrose (sugar) solution into an affected joint, which stimulates the body to repair connective tissue and strengthen the joint. It can be used to reduce pain and improve joint function. PRP is an injection of a concentrated solution of a person’s own platelets and blood plasma, which encourages the repair process of the affected joint.
Prolotherapy is an effective treatment for reducing pain and improving range of motion in TMJ dysfunction and has an excellent safety profile1-5. PRP is also been used to treat TMJ dysfunction and has been shown in several studies to improve the associated pain and limited range of motion6-10.
Both prolotherapy and PRP are safe, minimally invasive treatments and excellent options for people with TMJ dysfunction.
References
- Haggag MA, Al-Belasy FA, Said Ahmed WM. Dextrose prolotherapy for pain and dysfunction of the TMJ reducible disc displacement: A randomized, double-blind clinical study. J Craniomaxillofac Surg. 2022 May;50(5):426-431.
- Priyadarshini S, Gnanam A, Sasikala B, et al. Evaluation of prolotherapy in comparison with occlusal splints in treating internal derangement of the temporomandibular joint – A randomized controlled trial. J Craniomaxillofac Surg. 2021 Jan;49(1):24-28.
- Zarate MA, Frusso RD, Reeves KD, et al. Dextrose Prolotherapy Versus Lidocaine Injection for Temporomandibular Dysfunction: A Pragmatic Randomized Controlled Trial. J Altern Complement Med. 2020 Nov;26(11):1064-1073.
- Louw WF, Reeves KD, Lam SKH, et al. Treatment of Temporomandibular Dysfunction With Hypertonic Dextrose Injection (Prolotherapy): A Randomized Controlled Trial With Long-term Partial Crossover. Mayo Clin Proc. 2019 May;94(5):820-832.
- Mustafa R, Güngörmüş M, Mollaoğlu N. Evaluation of the Efficacy of Different Concentrations of Dextrose Prolotherapy in Temporomandibular Joint Hypermobility Treatment. J Craniofac Surg. 2018 Jul;29(5):e461-e465.
- Sousa BM, López-Valverde N, López-Valverde A, et al. Different Treatments in Patients with Temporomandibular Joint Disorders: A Comparative Randomized Study. Medicina (Kaunas). 2020 Mar 5;56(3):113.
- Fernández-Ferro M, Fernández-Sanromán J, Blanco-Carrión A, et al. Comparison of intra-articular injection of plasma rich in growth factors versus hyaluronic acid following arthroscopy in the treatment of temporomandibular dysfunction: A randomised prospective study. J Craniomaxillofac Surg. 2017 Apr;45(4):449-454.
- Hancı M, Karamese M, Tosun Z, et al. Intra-articular platelet-rich plasma injection for the treatment of temporomandibular disorders and a comparison with arthrocentesis. J Craniomaxillofac Surg. 2015 Jan;43(1):162-6.
- Pihut M, Szuta M, Ferendiuk E, et al. Evaluation of pain regression in patients with temporomandibular dysfunction treated by intra-articular platelet-rich plasma injections: a preliminary report. Biomed Res Int. 2014;2014:132369.
- Dasukil S, Arora G, Boyina KK, et al. Intra-articular injection of hyaluronic acid versus platelet-rich plasma following single puncture arthrocentesis for the management of internal derangement of TMJ: A double-blinded randomised controlled trial. J Craniomaxillofac Surg. 2022 Nov;50(11):825-830.