
What Is A Herniated Disc?
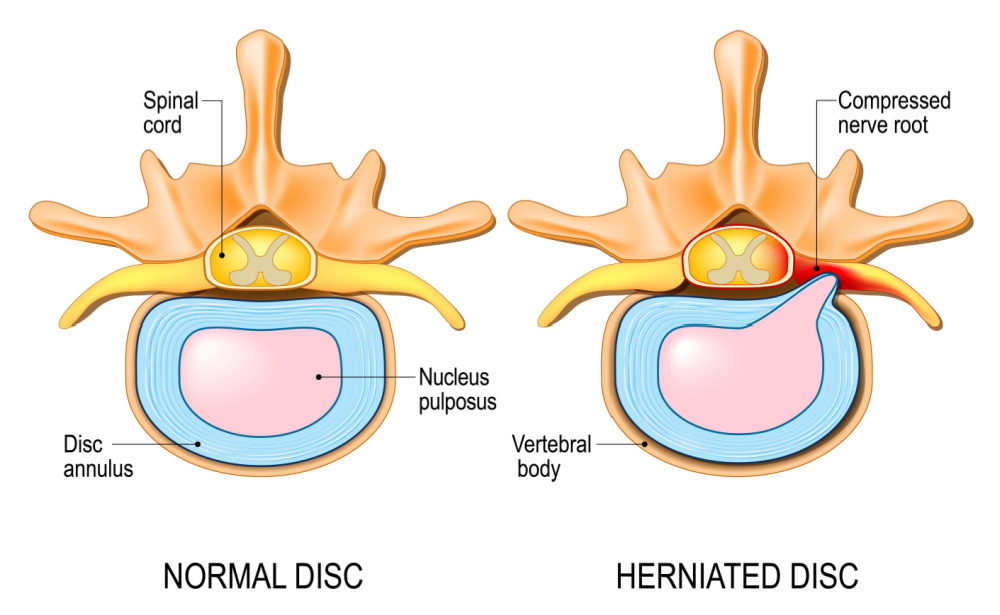
An intervertebral disc is made up of rigid, spongy tissue which sits between two vertebral bones (vertebrae) of our spine. This disc allows movement between two vertebrae and serves the important role of being a shock absorber. Mechanical forces that act on the spine are cushioned by the intervertebral discs, limiting excessive movement of the vertebrae, and protecting the spinal cord from damage. Each intervertebral disc is made up of two parts: a tough, rubbery outer portion called the annulus fibrosis; and a gelatinous, soft central portion called the nucleus pulposus.
When a disc is “herniated,” sometimes also referred to as “slipped,” “bulging,” or “ruptured,” it means that injury or degeneration to the outer portion of the disc has allowed for the inner portion to protrude out.
A herniated disc can occur at any level of the spine but the most commonly herniated discs are those in the lumbar spine (low back).
Symptoms Of A Herniated Disc
While not all cases of a herniated disc are painful, in some cases of significant compression of the spinal nerves, the pain can be severe. The protrusion of the disc can compress the nerve associated with its spinal level or even the spinal cord. Due to nerve involvement, herniated disc pain is often described as “burning,” “stinging” or “aching.” This pain can radiate into the lower extremity of the affected side (buttock, thigh, leg and/or foot) and can cause local muscle weakness or sensation changes in some cases. The pain associated with disc herniation is also contributed to by irritation caused by inflammation local to the disc protrusion.
Causes Of A Herniated Disc
The most common cause of disc herniation is degeneration due to aging. As humans age the nucleus pulposus dries and loses its structural integrity. In the case of degeneration, the disc herniation is progressive and without treatment will often worsen over time. The second most common cause of disc herniation is injury due to trauma. In these cases, the patient can usually recall when the injury occurred. Sports or activities that include heavy loads or repetitive flexion and rotation movements are often involved. (1)
Risk Factors For A Herniated Disc
People are most likely to have a symptomatic herniated disc between the ages of 30-60 and men are twice as likely as women. Between the ages of 25-55 approximately 95% of symptomatic herniated discs are either the L4-L5 or L5-S1 disc2 . While a herniated disc can cause severe pain, less than 5% of back pain is caused by a herniated disc3.
Research has determined a correlation between multiple lifestyle factors and the increased likelihood of suffering from disc herniation. Some of the most prevalent risk factors include:
- Obesity
- Smoking
- Sitting for long periods without standing or stretching
- Poor posture
- Lack of regular physical exercise4
Tests For A Herniated Disc
Most cases of symptomatic disc herniation will recover within a few weeks of injury. In office physical exams are performed to help rule in or out the diagnosis of a disc herniation. These tests include the straight leg test, femoral stretch test and valsalva maneuver. Neurological testing can also be done in-office to help determine the specific level of involvement (e.g.: muscle strength testing, deep tendon reflexes and sensory testing). However, imaging is indicated if a patient continues to display signs and symptoms of a herniated disc after 6 weeks. Magnetic resonance imaging (MRI) is the preferred imaging modality for identifying disc herniations5.
Conventional Treatment For A Herniated Disc
- Non-steroidal anti-inflammatory drugs
- Epidural corticosteroid injections
- Regular physiotherapy (beginning after at least 3 weeks of symptom onset).
- Surgical discectomy (removal of the herniated disc)6.
Naturopathic Treatment of A Herniated Disc
Rehabilitative exercise
Exercise based rehabilitation is an important part of the recovery process for many painful conditions, including a herniated disc. Strengthening of the paraspinal, abdominal and core muscles play a significant role in intervertebral disc herniation recovery7.
Acupuncture
In a meta-analysis performed on the use of acupuncture in the treatment of disc herniation acupuncture demonstrated a more favourable effect than ibuprofen and multiple other pain-relieving drugs8. In practice I have seen excellent results with acupuncture for herniated disc management in many cases.
Natural health products
Research has confirmed the role of various nutraceuticals in helping to prevent the degeneration of intervertebral discs and decrease associated inflammation9,10.
Prolotherapy
An integral part of the intervertebral disc herniation injury process is when the posterior longitudinal ligament fails and tears partially or undergoes a significant rupture. This ligament is the rigid structure which keeps the discs from herniating posteriorly (back) and then contacting the spinal nerves. The posterior longitudinal ligament is the last line of defence against a herniated disc.
Prolotherapy is a treatment used to repair ligament damage. This treatment involves injecting a concentrated sugar solution directly at the site of injury. The solution triggers an immune response, increasing local blood flow and stimulating the growth of healthy new ligament tissue. This has a strengthening effect on the ligament, providing increased support for the spine, helping to prevent further herniation, and reducing the chances of a recurrence of disc herniation.
Prolotherapy is also effective for treating the pain and disability associated with intervertebral disc herniation. Studies have shown that the strengthening effect of prolotherapy or platelet-rich plasma injections can reduce pain and improve mobility in patients with disc herniation11. Prolotherapy is also a safe, non-invasive procedure with minimal discomfort and a quick recovery time. For these reasons, prolotherapy is an increasingly popular treatment option for patients with disc herniation.
References
- Dydyk AM, Ngnitewe Massa R, Mesfin FB. Disc Herniation. In: StatPearls. Treasure Island (FL): StatPearls Publishing; January 18, 2022.
- Jordan J, Konstantinou K, O’Dowd J. Herniated lumbar disc. BMJ Clin Evid. 2009 Mar 26;2009:1118.
- Schwarzer AC, Aprill CN, Derby R, et al. The prevalence and clinical features of internal disc disruption in patients with chronic low back pain. Spine (Phila Pa 1976). 1995 Sep 1;20(17):1878-83.
- Zielinska N, Podgórski M, Haładaj R, et al. Risk Factors of Intervertebral Disc Pathology-A Point of View Formerly and Today-A Review. J Clin Med. 2021;10(3):409. Published 2021 Jan 21.
- Herniated disc. American Association of Neurological Surgeons. https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Herniated-Disc. Accessed July 30, 2021.
- Corniola MV, Tessitore E, Schaller K, et al. Hernie discale lombaire–diagnostic et prise en charge [Lumbar disc herniation–diagnosis and treatment]. Rev Med Suisse. 2014;10(454):2376-2382.
- Hahne, Andrew J. BPhysio; Ford, Jon J. PhD; McMeeken, Joan M. MSc. Conservative Management of Lumbar Disc Herniation With Associated Radiculopathy: A Systematic Review. Spine: May 15, 2010 – Volume 35 – Issue 11 – p E488-E504.
- Tang S, Mo Z, Zhang R. Acupuncture for lumbar disc herniation: a systematic review and meta-analysis. Acupunct Med. 2018;36(2):62-70.
- van Blitterswijk WJ, van de Nes JC, Wuisman PI. Glucosamine and chondroitin sulfate supplementation to treat symptomatic disc degeneration: biochemical rationale and case report. BMC Complement Altern Med. 2003;3:2.
- NaPier Z, Kanim LEA, Arabi Y, et al. Omega-3 Fatty Acid Supplementation Reduces Intervertebral Disc Degeneration. Med Sci Monit. 2019;25:9531-9537. Published 2019 Dec 14.
- Hauser RA, Matias D, Woznica D, et al. Lumbar instability as an etiology of low back pain and its treatment by prolotherapy: A review. J Back Musculoskelet Rehabil. 2022;35(4):701-712.